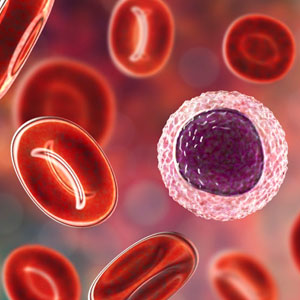
Blood Cancer
Blood cancer, also known as hematologic cancer or hematological malignancy, refers to cancers that affect the blood, bone marrow, or lymphatic system. These cancers typically involve abnormal growth and proliferation of blood cells or lymphocytes, which can interfere with the normal production and function of blood cells and immune cells. Blood cancers are broadly categorized into three main types: leukemia, lymphoma, and myeloma.
Types of Blood Cancer:
- Leukemia: Leukemia is a type of blood cancer that originates in the bone marrow and affects the production of white blood cells. There are four main types of leukemia:
1. Acute Lymphoblastic Leukemia (ALL)
2. Acute Myeloid Leukemia (AML)
3. Chronic Lymphocytic Leukemia (CLL)
4. Chronic Myeloid Leukemia (CML)
- Lymphoma: Lymphoma is a type of blood cancer that affects the lymphatic system, which includes lymph nodes, spleen, and lymphatic vessels. There are two main types of lymphoma:
1. Hodgkin Lymphoma (HL)
2. Non-Hodgkin Lymphoma (NHL) - Multiple Myeloma: Multiple myeloma is a type of blood cancer that affects plasma cells, which are a type of white blood cell responsible for producing antibodies. Multiple myeloma typically arises in the bone marrow and can lead to bone damage, anemia, and impaired immune function.
Risk Factors:
While the exact causes of blood cancer are often unknown, several factors may increase the risk of developing these cancers, including:
- Genetic Predisposition: Inherited genetic mutations or syndromes, such as Down syndrome, Li-Fraumeni syndrome, or familial predisposition to leukemia or lymphoma, may increase the risk of blood cancer.
- Exposure to Ionizing Radiation: Prolonged exposure to ionizing radiation, such as radiation therapy for a previous cancer or nuclear accidents, may increase the risk of developing leukemia or lymphoma.
- Chemical Exposure: Exposure to certain chemicals, such as benzene, pesticides, or industrial solvents, may increase the risk of developing blood cancer.
- Immune Suppression: Immunosuppressive conditions or therapies, such as HIV/AIDS, organ transplantation, or certain medications used to treat autoimmune diseases, may increase the risk of blood cancer.
- Viral Infections: Infections with certain viruses, such as Epstein-Barr virus (EBV), human T-cell lymphotropic virus (HTLV), or human herpesvirus 8 (HHV-8), may increase the risk of developing lymphoma.
Signs and Symptoms:
The signs and symptoms of blood cancer vary depending on the type and stage of the cancer but may include:
- Persistent fatigue, weakness, or lethargy.
- Unexplained weight loss or loss of appetite.
- Frequent infections or illnesses.
- Easy bruising or bleeding.
- Swollen lymph nodes, particularly in the neck, armpits, or groin.
- Night sweats or fevers without an apparent cause.
- Persistent or unexplained bone pain.
- Enlarged liver or spleen.
- Shortness of breath or chest pain (in cases of mediastinal lymphoma).
- Neurological symptoms, such as headaches, seizures, or vision changes (in cases of central nervous system involvement).
Diagnosis and Treatment:
Diagnosing and treating blood cancer often requires a multidisciplinary approach involving hematologists, oncologists, pathologists, and other healthcare professionals. Diagnostic tests may include blood tests, bone marrow biopsy, imaging studies (such as CT scans or PET scans), and molecular or genetic testing.
Treatment options for blood cancer depend on various factors, including the type, stage, and molecular characteristics of the cancer, as well as the patient's age and overall health. Common treatment modalities may include chemotherapy, targeted therapy, immunotherapy, radiation therapy, stem cell transplantation, and supportive care services.
Prognosis:
The prognosis for blood cancer varies depending on the type and stage of the cancer, as well as individual factors such as the patient's age, overall health, and response to treatment. Advances in research and clinical care have led to significant improvements in survival rates for many types of blood cancer, with some patients achieving long-term remission or even cure.
Support and Survivorship:
Blood cancer diagnosis and treatment can have significant physical, emotional, and psychosocial effects on patients and their families. Comprehensive supportive care services, including psychosocial support, pain management, nutritional support, and rehabilitation services, are essential components of blood cancer care. Additionally, survivorship programs provide long-term follow-up care and support for blood cancer survivors, addressing potential late effects of treatment and promoting overall health and well-being.
In summary, blood cancer is a complex and diverse group of diseases that require specialized care and treatment. Advances in research and clinical care continue to improve outcomes and quality of life for patients with blood cancer, highlighting the importance of early detection, timely intervention, and comprehensive supportive care.



